By Abujah Racheal, News Agency of Nigeria (NAN)
Mr Shedreck Hammayaji, 37-year-old, a dedicated nurse at Kwali General Hospital, Kwali, Abuja, demonstrates an unwavering commitment to healthcare and community service despite facing numerous challenges.
During the height of outbreaks, Hammayaji said that he witnessed the strain on the healthcare system firsthand as patients inundated the hospital with symptoms of the deadly virus.
“I remember the fear in people’s eyes as they sought treatment, unsure if they would survive.
“We were overwhelmed, with limited supplies and staff to handle the growing number of cases,” he recalled.
His experiences shed light on the critical importance of adequate funding in epidemic preparedness.
With increased resources, healthcare workers like him could receive better training, access essential equipment, and strengthen disease surveillance systems to respond effectively to outbreaks.
His story serves as a poignant reminder of the profound impact of funding decisions on frontline healthcare workers and the communities they serve.
It underscored the urgent need to invest in epidemic preparedness to safeguard the health and well-being of Nigerians nationwide.
In light of recent health crises also unknown in the country, including outbreaks of diphtheria, Lassa fever, measles, and meningitis, the significance of epidemic preparedness funding cannot be overstated in Nigeria.
Nigeria, as one of the most populous countries in Africa, faces unique challenges in dealing with potential epidemics due to its large and diverse population.
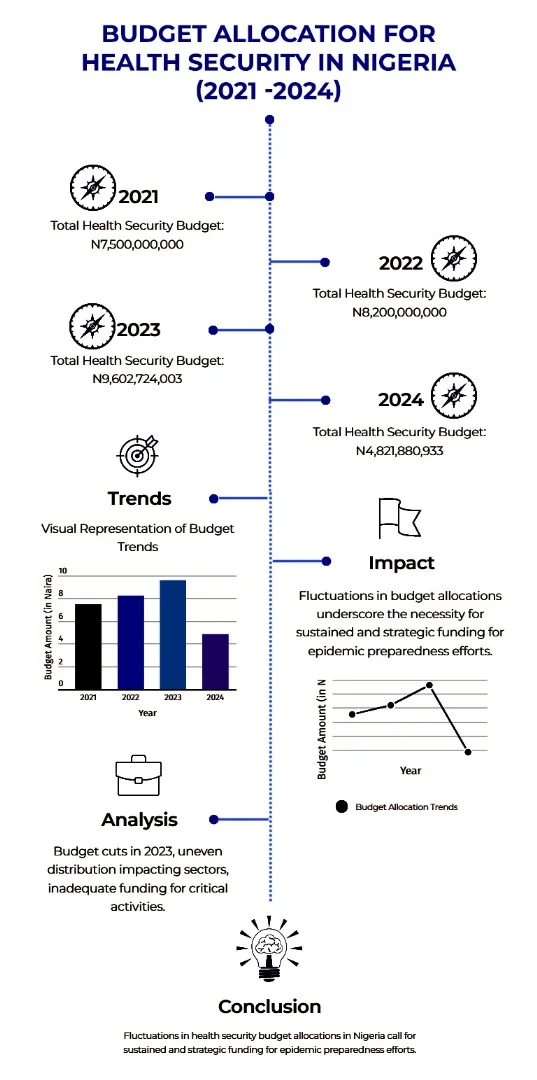
Comparing the budget amounts for 2024 with the total budget for health security in 2023 reveals a significant discrepancy.
The Ebola outbreak in West Africa stands as one of the deadliest in history, starkly illustrating the repercussions of insufficient epidemic preparedness funding.
The impact was profound: limited funding impeded early detection and response efforts, exacerbating the severity of the outbreak.
Conversely, countries with stronger healthcare systems and better-funded preparedness programmes demonstrated more effective responses.
Beyond the human toll, the outbreak inflicted economic turmoil, especially in regions lacking adequate preparedness funding, resulting in income loss and trade disruption.
Despite global mobilisation, the fragmented response underscored the urgent need for enhanced coordination and investment in preparedness.
From this crisis emerged valuable lessons- the critical necessity of adequate funding for preparedness to mount effective outbreak responses.
Moreover, it highlighted the pivotal role of public-private partnerships and international cooperation in shaping an effective response framework.
According to public health experts, investing in preparedness not only fortifies healthcare systems but also equips them to confront future threats with resilience.
In spite of commendable strides in recent years, they said that the country still faces significant challenges in funding epidemic preparedness, as per a recent World Health Organisation (WHO) report.
The report underscores the need for increased investment in surveillance, laboratory capacity, and health system strengthening to adequately respond to infectious diseases.
One major challenge the report said was the lack of sustained financial commitment from both the federal government and international donors.
While funding spikes during crises like the Ebola outbreak and the COVID-19 pandemic, it often lacks consistency, hindering long-term preparedness efforts.
The COVID-19 pandemic also exposed the vulnerabilities in the country’s health system, underlining the urgent need for increased investment in epidemic preparedness.
Shortages of critical supplies during the pandemic highlighted the consequences of insufficient funding allocation and prioritisation.
To address these challenges, experts underscored coordinated efforts to prioritise preparedness, boost funding commitments, and enhance resource allocation and utilisation.
The Joint External Evaluation (JEE) tool has been instrumental in evaluating Nigeria’s health capacities, leading to notable improvements in health security ratings.
Nigeria utilised the JEE tool 3.0 to evaluate the implementation status of health capacities in the country, measuring progress across 56 indicators spanning 19 International Health Regulations (IHR) core capacities.
Dr Geoffrey Jagero, Senior Technical Advisor for Laboratory Systems at the Division of Global Health Protection, US CDC Kenya, stressed the importance of increasing trained professionals in biological risk management.
Jagero called for collaboration with government agencies to develop biosecurity frameworks.
Dr Patrick Nguku, AFENET Regional Technical Coordinator, stressed the need for investment in healthcare infrastructure, disease surveillance systems, and training healthcare workers for early detection and reporting.
Dr Solomon Chollom, a Virologist, highlighted the importance of collaboration between Nigeria and international donors through joint funding mechanisms, advocacy efforts, and transparent fund utilisation.
Dr Gafar Alawode, Chief of Party, Health Financing Governance Projects, advocated for public-private partnerships to bolster epidemic preparedness funding, diversifying funding sources through innovative mechanisms like social impact bonds.
Alawode stressed the urgency of bolstering epidemic preparedness financing mechanisms, addressing bureaucratic inefficiencies, and strengthening domestic resource mobilisation.
Meanwhile, Dr Simeon Onyemaechi, Chairman of the Forum of CEOs of State Social Health Insurance Agencies (SSHIA), emphasised the necessity of adopting a holistic approach to address the funding gap in epidemic preparedness.
Onyemaechi highlighted the importance of prioritising collaboration among stakeholders, implementing innovative financing mechanisms, and enacting policy reforms to strengthen Nigeria’s preparedness efforts.
The Coordinator, Africa Health Budget Network, AHBN, Dr Aminu Magashi, said that the country needs more funding to pay hazard allowances on a monthly and timely basis to the teeming frontline health workers such as medical doctors, nurses, laboratory technicians amongst others.
Magashi said that as of now, payment was erratic and meagre and not commensurate to the risk of exposure to infections.
He stressed the urgent need for governments to fortify healthcare systems and improve surveillance and response mechanisms for infectious diseases.
He emphasised the importance of domestic financing for health initiatives while also advocating for ongoing international support.
In conclusion, investing in epidemic preparedness is essential for Nigeria’s resilience to health emergencies and sustainable development.
By examining funding mechanisms, identifying gaps, and implementing strategic interventions, Nigeria can ensure a healthier future for its citizens. (NANFeatures)
**If used please credit the Writer and News Agency of Nigeria (NAN)